Infertility is the absence of pregnancy for any reason after 1 year of sexual activity without the use of contraceptive methods or after 6 months if the woman is over 35 years old. According to Rosstat, more than 3% of women in Russia who are of reproductive age (from 20 to 44 years old) suffer from infertility after the first birth, and almost 2% are not able to give birth at all.
There are many reasons that interfere with conception or gestation: from health problems to psychological factors. Male infertility can also occur, but due to the complexity of the female reproductive system, most infertile marriages are associated with malfunctions in the woman's body. In most cases, the cause of the absence of pregnancy can be identified and corrected with medication or surgery, but unidentified factors also occur.
The normal process of reproduction requires the interaction of male and female germ cells. During the release of the egg from the ovaries, it then moves through the fallopian tubes to the uterus. The male reproductive organs produce sperm.
The sperm and egg usually meet in the woman's fallopian tube where fertilization takes place. The embryo is implanted in the uterine cavity for further development. Female infertility is when, for some reason, this circuit fails.
The most common problems leading to infertility are:
- violations of the ovulation process (in 36% of cases);
- (30%);
- endometriosis (18%);
- Unknown causes of infertility remain in 10% of women.
Hormonal infertility
A delicate balance of female sex hormones (estrogen, progesterone, luteinizing hormone, follicle-stimulating hormone) is necessary for the timely maturation and release of the egg from the ovary.

The following hormonal disorders can cause infertility:
- Polycystic ovaries. Due to an excess of male hormones or hypersecretion of insulin by the pancreas, many follicles form in the ovaries, but none of them mature and release an egg, that is, ovulation does not occur. The ovaries increase in size up to 2-6 times, the monthly cycle lengthens, some periods may be missed. 70% of women diagnosed with PCOS are overweight.
- Resistance (resistance) to insulin, often associated with polycystic disease. The hormone insulin, produced by the pancreas, is responsible for delivering sugar from the blood to the body's cells. If the cells stop taking it, more insulin is released in response to the increase in blood sugar. According to studies, resistance is associated with an increased number of male genital organs - hyperandrogenism. The causes of cell resistance to insulin are malnutrition, stress, and a sedentary lifestyle.
- Increased amount of male hormones. Irregular or even absent periods may indicate hyperandrogenism. Excess male hormones suppress the functioning of the ovaries, up to the cessation of ovulation and lead to infertility. Hyperandrogenism also causes a strong growth of body hair, acne, a coarsening of the voice and a change in the male figure.
- An excess of the hormone prolactin produced by the pituitary gland (hyperprolactinemia). Problems in the functioning of the gland occur due to impaired blood supply, genetic causes, injuries, medication, and meningitis. Characteristic signs of the disease are the appearance of milk in the breast and violations of the monthly cycle. Mastopathy, growth of the mammary glands, bone fragility, and a decrease in sexual desire are also observed. Prolactin is a hormone of nursing mothers, it is because of it that many of them do not ovulate and menstruate. An increase in this hormone in other women is usually associated with thyroid dysfunction (hypothyroidism).
- Premature menopause. The average age of onset of menopause is 50 years, but due to autoimmune or genetic disorders, diseases of the reproductive system, unhealthy lifestyle, smoking and other reasons, 1% of women experience menopause before the age of 40. The production of female hormones decreases, ovarian function and fertility gradually fade away.
- Insufficiency of the corpus luteum. The corpus luteum is a temporary gland that occurs instead of the follicle that released the egg. The hormone of the gland, prolactin, stimulates the preparation of the uterus for fixing a fertilized egg in it. If it is not enough, fixation does not occur and pregnancy does not occur, but if implantation occurs, a miscarriage soon occurs. Conditions of insufficiency of the corpus luteum - genetic disorders, ovarian pathologies (polycystic ovary syndrome, cancer), malfunctions of the pituitary gland.

Physiological factors of infertility
- Damage to the fallopian tubes or lack of patency. It is in the fallopian tubes that fertilization takes place after the release of the egg from the ovary and connection with the spermatozoon, therefore, if they are obstructed, fertilization is impossible. The tubes can be damaged as a result of inflammation, after viral or bacterial infections, sexually transmitted diseases, complications from surgery, when adhesions or scarring occur.
- Endometriosis. Due to genetic factors, the pathology of immune and hormonal processes, the uterine mucosa forms in inappropriate places inside and outside the reproductive tract. Endometriosis can block the fallopian tubes and prevent ovulation, leading to infertility. Signs of this disease are pain, heavy and painful periods.
- Myoma of the uterus. It is believed that the cause of fibroids (a benign growth on the uterus, consisting of muscle tissue) is an increase in estrogen levels. Risk factors - genetic predisposition, metabolic disorders, stress, abortion. Myoma makes itself felt with the help of heavy menstruation, cycle disorders, pain. The consequences of the appearance of a tumor depend on its size and location, in some cases it causes infertility, miscarriages or pregnancy complications.
- Adhesions and anomalies in the shape of the uterus (one-horned and two-horned, the presence of a septum, uterine infantilism). The cause of adhesions and fusion of the walls of the uterus are inflammatory processes, trauma and endometriosis, and structural pathologies are caused by genetic causes. The consequence of these problems is most often spontaneous abortion, since the fertilized egg cannot gain a foothold in the uterus.
- Scarring of the cervix or abnormalities of its shape. Adhesions and scars on the cervix - a consequence of surgery or infection. Because of this, spermatozoa do not pass into the fallopian tubes and infertility occurs. A deformity of the cervix or changes in the composition of the cervical mucus can also make it difficult for sperm to travel.
- Inflammation of the pelvic organs. The reason for this may be infections caused by several types of bacteria, in particular, sexually transmitted infections (STDs) - gonorrhea, chlamydia, ureaplasmosis, and many others. Factors that increase the risk of infection are sex without a condom and changing sexual partners. Pathogenic bacteria can enter the body during intrauterine manipulations, during menstruation, in the postpartum period, since at this time the effectiveness of natural defense mechanisms decreases. Infections can cause inflammation of the tubes and ovaries (salpingoophoritis) in combination with inflammation of the uterus (endormetritis), as well as inflammation of the cervix (cervicitis). The disease is characterized by abdominal pain, unusual discharge (including uncharacteristic periods), sores, spots, itching, and soreness of the genitals.

Other factors
- Age. By the time of puberty, a woman's ovaries contain about 300,000 eggs. Over time, they age - DNA is damaged, since the system for its restoration works worse with age. Accordingly, their quality decreases - suitability for fertilization and development of the embryo. This process becomes noticeable after 30 years, and when a woman turns 35-40, aging accelerates.
- Overweight or underweight. An excess amount of adipose tissue in the body threatens hormonal disruptions - an increase in the amount of estrogen and testosterone, which threatens gynecological diseases up to infertility. Obese women may become pregnant under the influence of drugs, but often there are problems with the bearing and development of the child. Underweight (BMI less than 18.5) also leads to disruption of the endocrine system, but hormones are produced less than necessary for the normal functioning of the reproductive system, eggs stop maturing.
- Stress, nervous exhaustion, chronic fatigue. Stress is the cause of hyperprolactinemia and a decrease in the level of estrogen in the blood, which affects the possibility of maturation of the egg and its attachment to the uterine wall. Another consequence of emotional overload is spasms and muscle contractions, which leads to hypertonicity of the uterus and fallopian tubes, which prevents conception.
- congenital disorders. Stein-Leventhal syndrome (provokes polycystic ovary syndrome), adrenogenital syndrome (impaired functioning of the adrenal glands and increased levels of androgens), Shereshevsky-Turner syndrome (absence of menstruation), bleeding disorders and some other disorders are of a genetic nature and interfere with conception or cause early miscarriages.
- Immunological factors. The presence of anti-sperm antibodies in the cervical mucus can lead to infertility. In other cases, the mother's immune system prevents the embryo from attaching to the uterine wall and thus causes a miscarriage.
- psychological reasons. In some cases, a woman subconsciously perceives pregnancy as a danger. This can be caused by moral trauma, fear of changes in life or appearance, fear of childbirth. The brain controls all processes in the body, so a negative psychological attitude leads to infertility.
Types of female infertility
There are several types of infertility, differing in conditions and mechanism of occurrence.
Depending on the possibility of eliminating the causes that caused problems with conception, and the chances of a subsequent pregnancy, there are:
- relative infertility, when after taking medication, normalizing hormonal levels or metabolism, surgery to restore reproductive function or other treatment, conception can occur;
- absolute, in this case, due to congenital factors, incurable diseases or disorders, a natural pregnancy is impossible.
In some cases, after the first pregnancy (successful or unsuccessful), a woman cannot conceive again for various reasons, but often the first pregnancy does not occur. Depending on this, there are:
- primary infertility (lack of pregnancy);
- secondary infertility (there are cases of pregnancy in the anamnesis).
According to the mechanism of occurrence:
- acquired infertility occurs due to injuries, infections, diseases of the reproductive and endocrine systems that are not associated with a genetic factor;
- congenital - hereditary diseases, developmental anomalies.
For the reasons that caused it, infertility is divided into the following types:
- tubal (associated with obstruction of the fallopian tubes);
- endocrine (caused by disorders of the endocrine glands);
- infertility due to uterine pathologies;
- peritoneal, when adhesions in the pelvic organs interfere with conception, but the fallopian tubes are passable;
- immunological infertility is caused by the formation of antibodies to sperm in the female body;
- infertility due to endometriosis;
- idiopathic (of unknown origin).
Diagnosis of infertility in women

The causes of female infertility are varied, often to find out it is necessary to undergo a large number of examinations.
To diagnose the presence and cause of female infertility, a consultation with a gynecologist or reproductologist is necessary. He should find out from the patient whether she has complaints about pain, discharge, the duration of unsuccessful attempts to get pregnant, the presence of genetic or infectious diseases, surgeries, complications, the nature of menstruation and sexual life. Also, the doctor performs an examination both external - to assess the physique, the presence of excess body hair, skin condition, and gynecological, including checking the condition of the internal genital organs.
There are a number of functional tests offered to determine the causes of infertility:
- cervical index, which involves the evaluation of cervical mucus to determine the level of estrogens;
- building a basal temperature curve, which allows you to evaluate the fact and time of ovulation;
- postcoital test, when the activity of spermatozoa in the cervix is studied and the presence of antibodies to sperm is established.
To find out the causes of infertility, the following tests are offered:
- For laboratory diagnosis of infertility, the hormonal background is first checked. In particular, this is an assessment of the level of testosterone, prolactin, cortisol on day 5–7 of the cycle, progesterone on day 20–22, hormonal tests, when indicators are evaluated after stimulation or inhibition of various hormonal processes based on their response.
- An STD test is mandatory.
- The study of the content of antibodies to sperm in the blood and cervical mucus is an immunogram, analysis of vaginal secretions and compatibility tests.
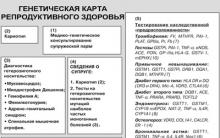
- Genetic analysis of chromosomal abnormalities leading to infertility.
The woman will be asked to undergo the following examinations:
- ultrasound. Allows you to see violations of the pelvic organs, uterine fibroids, assess the structure of the uterus, ovaries, fallopian tubes and their patency. You can also evaluate the processes of ovulation and maturation of follicles.
- Hysterosalpingography (HSG)- Examination of the internal genital organs using x-rays. The contrast agent injected by the gynecologist gives an informative picture of the state of the uterus, fallopian tubes, and ovaries.
- Skull x-ray, since the cause of infertility may be a malfunction of the pituitary gland or its tumor.
- Colposcopy, including examination of the vagina and cervix by introducing a colposcope - a special device consisting of a binocular and a lighting device. This study allows you to identify signs of erosion and cervicitis - signs of the inflammatory process.
- Hysteroscopy. It is performed under general anesthesia using an optical instrument of a hysteroscope inserted through the vagina. It makes it possible to visually assess the cervical canal, uterine cavity, fallopian tubes, and also take the uterine mucosa for analysis.
- Laparoscopy- This is a check of the pelvic organs with optical equipment through a micro-incision on the abdomen. Like hysteroscopy, this is a low-traumatic operation, after 1-3 days the patient can leave the hospital.
Treatment of infertility in women
The decision on the methods and the need for treatment is made after all examinations and the establishment of the causes of infertility. If it is relative, therapeutic or surgical methods of treatment are used, absolute (incurable) infertility requires alternative solutions to the problem - assisted reproductive technologies.
Medical treatment
Infertility drugs are mainly prescribed to correct ovulation disorders in patients due to hormonal problems. This method is used as the first treatment option for many patients, often used after surgery or in combination with IVF and ICSI.

There is a wide range of drugs. The most common ones are:
- Clomid and Serofen. These drugs are taken in the form of tablets and stimulate the process of ovulation, forcing the production of hormones necessary for the maturation of the egg, the hypothalamus (gonadotropin hormones) and the pituitary gland (follicle-stimulating and luteinizing hormones).
- Hormone injections: human chorionic gonadotropin (hCG), follicle stimulating hormone (FSH), human menopausal gonadotropin (hMG), gonadoliberin (Gn-RH), gonadoliberin agonist (GnRH agonist). Hormones are given by injection at regular intervals. These drugs are more effective and more expensive than Clomid and Serofen. They are generally used to induce ovulation and subsequent IVF.
- Utrozhestan- a drug containing progesterone and stimulating the preparation of the uterus for egg implantation.
- Duphaston due to the content of dydrogesterone, it helps the fertilized egg to attach to the uterus.
- Bromocriptine inhibits the production of prolactin.
- Wobenzym It is prescribed for inflammations and infections, as it increases the body's resistance.
- Tribestan normalizes the level of estrogen and follicle-stimulating hormone.
Surgery
Surgery can solve a number of issues, but it is used only in the initial stage of infertility treatment for several reasons.
These can be the following types of operations:
- Removal of polyps, fibroids, cysts Removal of excess or abnormal tissue in the uterine or ovarian cavity can improve ovulation and clear the way for sperm and egg to reunite. The excised tissues are always sent for biopsy to check for malignant cancers.
- Surgical treatment of endometriosis. The operation is prescribed when conservative methods of infertility treatment do not help, and the disease leads to severe pain and disruption of the urinary system.
- Restoration of ligated fallopian tubes. For sterilization purposes, women's fallopian tubes may be cut or soldered. The reverse process - the restoration of their patency - is a serious surgical operation, the successful outcome of which depends on the method and prescription of blocking the pipes and their condition.
- Salpingolysis- removal of adhesions on the fallopian tubes.
- Salpingostomy- to restore the patency of the fallopian tube, the area with impaired patency is removed, and the remains of the tube are connected.

These operations are performed using hysteroscopy or laparoscopy, but when removing large cysts, fibroids, extensive endometriosis, a laparotomy is used when a large incision is made on the abdomen.
Assisted Reproductive Technologies (ART)
In ART, an egg is fertilized by a sperm outside the body. The ART procedure is based on the surgical removal of an egg from the ovaries, combining it with sperm in the laboratory and returning it to the patient's body or transplanting it to another woman. Mostly in vitro fertilization (IVF) is used.
The success of the operation varies depending on many conditions, including the cause of infertility and the age of the woman. According to statistics, after the first IVF protocol, pregnancy occurs in 40% of women under the age of 35 and gradually decreases to 2% in those over 44 years of age.
ART can be expensive (only free IVF is covered by the CHI policy) and time-consuming, but it allows many couples to have children.
Types of ART:
- ECO- the most effective and common form of ART. With the help of drugs, superovulation is caused in a woman (the maturation of several eggs), which are then combined with the man's sperm under special conditions, and after fertilization they return to the patient's uterus. The seed material may belong to the husband, or it may be donor - cryopreserved.
- ICSI(Intra Cytoplasmic Sperm Injection - intracytoplasmic sperm injection) is often used for couples with male factor infertility. One healthy sperm is placed in the egg, unlike IVF where they are placed in a petri dish together and fertilization occurs on its own.
- Embryo transfer (gametes) into the fallopian tubes- GIFT and ZIFT. The embryo is transferred into the fallopian tubes instead of the uterus.
- Insemination with husband's sperm (IMS) or insemination with donor's sperm (IDS) is used when vaginal ejaculation is impossible, "bad" spermatozoa, the use of cryopreserved seminal material. Spermatozoa are transferred into the vagina or directly into the uterine cavity.
- Surrogacy offered to women who do not have a uterus. The patient's egg is fertilized with the husband's sperm and transferred to the uterus of a surrogate mother - the woman who will bear the child.

Complications in the use of ART can be an allergy to drugs for stimulating superovulation, ovarian hyperstimulation syndrome, inflammation and bleeding.
If, as a result of long treatment and numerous attempts to have a child, including using assisted reproductive methods, pregnancy does not occur, do not despair. Those couples who are confident in their desire to have a child may consider adoption.
The adoption process requires the collection of a large number of documents and often a long selection of candidates. There are also risks of ignorance about the genetic characteristics of the child or lack of understanding if an older child is adopted, so such a decision requires a balanced approach.
In order to conceive and bear a child, a woman needs healthy ovaries, fallopian tubes, uterus, endocrine system. Disruption of any of these organs can contribute to infertility. It is wise to seek medical attention if risk factors are present - irregular menstruation, endometriosis, ectopic pregnancy, PCOS, pelvic inflammatory disease, and others.
To establish the causes of infertility, a lot of tests and examinations are required, including studies for hormonal and genetic disorders, the search for pathologies of the genital organs and infectious diseases. In most cases, infertility can be cured with medication (mainly hormonal agents), surgery, or assisted reproductive technology. The latter give a chance to those couples who, due to health problems, are unable to have children naturally.
Olga Rogozhkina
midwife
If within 12 months a woman has not become pregnant with regular unprotected intercourse, then she is diagnosed with infertility. Why is this time allotted for a possible conception? The 12-month period is clarified by statistics: it has been proven that 30% of women were able to become pregnant in the first 3 months of open sexual activity, 60% - over the next 7 months, 10% - after 11-12 months from the start of pregnancy planning. It turns out that one year is enough to confirm the fertility of a woman. Modern medicine is able to solve the issue of female infertility in most situations. A reproductive specialist helps to identify the type of infertility and choose options for solving this problem.
Useful video about solving the problem of female infertility
I like!
An important step before starting hormonal treatment aimed at restoring the correct hormonal balance in a woman's body is the mandatory determination of the cause of certain disorders and the solution of the issue of identifying contraindications to this type of treatment. In our clinic, for the competent management of such patients, gynecologists-reproductologists and endocrinologists necessarily interact to achieve the maximum effect of the therapy! With us you can quickly undergo an examination of any degree of complexity for the diagnosis of endocrine (hormonal) infertility and get a consultation from a specialist doctor based on the results of the tests!
Hormonal treatments for infertility are widely used to normalize the work of the endocrine (hormonal) system of a woman's body and normalize reproductive function and include three main areas:
- Normalization of the functions of the endocrine system, which restores the work of the adrenal glands, thyroid gland and other organs responsible for the production of important hormones involved in the regulation of the woman's menstrual cycle. Most often, when examining patients with infertility, a reproductive specialist has to deal with a change in the indicators of substances that can affect the process of ovulation, and hence the onset of pregnancy. These biologically active substances include prolactin, which is produced in the central nervous system by the cells of the anterior pituitary gland. An increase in prolactin can lead to anovulatory (lack of ovulation and the release of an egg from the ovary) infertility or miscarriage. In this case, therapy with drugs such as bromocriptine, cabergoline, quinagolide and others can be prescribed. An important point in preparing for pregnancy is to identify an insufficient balance of thyroid hormones, in connection with which hormonal preparations containing thyroid hormones (euthyrox, L-thyroxine) come to our aid. Regulation of the adrenal glands also requires, in some cases, the appointment of hormonal preparations in cases of increased levels of androgens (male hormones) in the blood of a woman, with diseases such as dysfunction of the adrenal cortex.
- Replacement of the hormonal function of the ovaries in case of their insufficient work, and consequently a decrease in the production of hormones. Hormone replacement therapy is prescribed for conditions such as ovarian failure syndrome, menstrual irregularities, accompanied by insufficient growth of the endometrium or insufficient production of the main female hormones progesterone and estrogen. The appointment of drugs containing these active biological substances leads to the normalization of hormonal balance.
- Stimulant, aimed at stimulating ovarian function. The purpose of such therapy is to restore the processes of maturation of the follicle, to activate ovulation - the release of the egg from the ovary.
Indications for ovarian stimulation
- With infertility caused by the absence of ovulation (violation of the release of an egg from the ovary), not amenable to treatment for more than 1 year up to 30 years and more than 6-8 months over 30 years.
- In the absence of pregnancy after surgical treatment for 6 months (PCOS, external genital endometriosis).
Conditions for holding
- Evaluation of the patency of the fallopian tubes with the help of ECHO-GSS (hysterosalpingography), X-ray of the GSS (the conclusion on the confirmation of their patency is not more than 1 year old);
- Confirmation of the absence of a mature follicle (17 mm or more in diameter) on days 11-16 of the cycle or the absence of a corpus luteum on days 19-23 of the cycle.
- Determination of the level of hormones on the 2nd-3rd day of the menstrual cycle (TSH-thyroid-stimulating hormone, FSH-follicle-stimulating hormone, LH-luteinizing hormone, testosterone, DHEA-S, 17-OP-hydroxyprogesterone, estradiol, prolactin), progesterone levels at 18-23 - day of the cycle;
- Detection of the LH peak preceding ovulation using home urinary ovulation tests (Kliaplan, EVITEST, Frautest, Clearblue test) on the 11-16th day of the cycle.
- Absence of malignant neoplasms;
- Absence of acute inflammatory diseases of the pelvic organs and exacerbation of chronic forms at the time of stimulation;
- The absence of exacerbation of chronic diseases of other body systems at the time of the onset of stimulation of ovarian function;
- No problems with the patency of the fallopian tubes and the thickness of the mucous membrane of the uterine cavity.
Options for achieving pregnancy against the background of hormonal stimulation of ovarian function
- Ovulation induction (programmed conception). The appointment of drugs that stimulate the growth of the follicle, the introduction of drugs that cause ovulation, and the determination of the most favorable days for conception;
- Ovulation induction combined with artificial insemination with husband's or donor's sperm. With the combined use of clomiphene citrate and urinary gonadotropins for ovarian stimulation, compared with the natural cycle, the efficiency of pregnancy increases from 4.3% to 18.8%; according to foreign authors, up to 21.6%.
Groups of drugs used to stimulate ovarian function
- Antiestrogens (clomiphene citrate-clomid, clostilbegit) 25mg, 50mg, 100mg;
- Gonadotropins;
- Human menopausal gonadotropins (HMG) (containing FSH and LH), eg Menopur containing FSH 75 IU and LH 75 IU;
- Human chorionic gonadotropins (HCG) example, Horagon, Pregnyl (1500 IU, 5000 IU);
- Recombinant gonadotropins (higher degree of purification, no risk of infectious complications) rFSH preparations, example Gonal-F (75, 150 IU, etc.).
Indications for clomiphene citrate
- Age up to 30 years
- Irregular menstruation for up to 5 years
- Duration of infertility no more than 2 years
- Menstrual irregularity
- No signs of ovulation on pelvic ultrasound and urinary ovulation tests.
- Before taking the drug, it is recommended to examine the function of the liver, due to the fact that the metabolism of the drug is associated with the work of this organ.
- The drug should not be prescribed to women without a preliminary hormonal examination, gynecological examination and exclusion of diseases of such organs as the thyroid gland, adrenal glands, pituitary gland (brain).
- Before starting the use of the drug, all other causes of infertility that are not associated with ovulation disorders should be eliminated.
- If ovarian enlargement or cystic changes occur while taking the drug, treatment should be discontinued until the size of the ovaries returns to normal. In the future, the reception can be resumed, but at the same time reduce the dose of the drug or the duration of treatment.
- When using clostilbegit, ultrasound monitoring or folliculometry is necessary, which allows to estimate the size of the dominant follicle in the ovary and fix the process of completed ovulation.
- Drug stimulation of ovulation increases the likelihood of multiple pregnancy.
- The appointment of the drug should be made with caution or replaced by other drugs, women with galactose intolerance, lactase deficiency or glucose malabsorption, tk. each tablet contains 100 mg lactose.
- This medicine affects the ability to drive vehicles and control mechanisms, due to the potential effect on the organs of vision.
The problem of infertility is becoming especially relevant in the modern world. Many negative factors affect the human reproductive system. Even during intrauterine development, the genital organs of the fetus are exposed to pathological influences through the mother's blood (tobacco smoke, medication, unbalanced diet, infections). Further, the negative influence of the environment only intensifies. The number of so-called “barren marriages” is on the rise all over the world. The World Health Organization calls this a marriage where a woman does not become pregnant within a year of regular sexual life without contraception. One of the main ones is the hormonal factor. So in women, endocrine disorders are the cause of infertility in 35-40% of all cases, and in men - in 8-12%.
Hormonal infertility in women Hormonal infertility in women is based on a violation of the ovulation process. Normally, in a non-pregnant woman of childbearing age, an egg matures in the ovaries every month. Further, fertilization and the onset of pregnancy can occur. The absence of ovulation (anovulation) occurs when the process of selection, growth and maturation of the dominant follicle in the ovaries is disrupted. The ovaries change their normal structure to polycystic (multifollicular). Such ovaries begin to produce an excess amount of androgens (male sex hormones), and the overall production of sex hormones decreases. Anovulation occurs in polycystic ovary syndrome, adrenogenital syndrome, hyperprolactinemia, hypothyroidism, hypogonadotropic hypogonadism, insufficiency of the hormonal function of the corpus luteum.
Diagnosis of hormonal infertility
Anovulation and, accordingly, infertility can occur with a regular menstrual cycle, but are more often observed in the form of a prolonged absence of menstruation. Basal body temperature during the month remains monotonously low. Dominant follicles and corpus luteum are not found on ultrasound. Hormonal examination in a woman most often reveals normal levels of pituitary hormones: FSH (follicle-stimulating) and LH (luteinizing). There is no LH peak in the middle of the cycle. Depending on which disease led to the development of anovulation, disturbances from other hormones may be detected. In hypothyroidism, a high level of thyroid-stimulating hormone (TSH) and a decrease in thyroid hormones (T4 and T3) are found. With hyperprolactinemia, an increase in prolactin in the blood is detected. Hypogonadotropic hypogonadism is characterized by low levels of FSH, LH, estradiol.
Diagnosis of hormonal causes of infertility is carried out jointly by a gynecologist and an endocrinologist. Particular attention is paid to the most common pathology - polycystic ovary syndrome, hypothyroidism, hyperprolactinemia. Hormonal examination is prescribed several times during the menstrual cycle. Ultrasound diagnosis is also recommended at least twice. Ultrasound of the thyroid gland, adrenal glands, computed or magnetic resonance imaging of the pituitary gland may be needed.
Treatment of hormonal infertility
Hypothyroidism is treated with thyroid hormones (usually L-thyroxine). If prolactinoma has become the cause of infertility, conservative therapy (currently most often cabergoline) or an operative method of treatment is selected. In the event that hormonal infertility is a consequence of adrenogenital syndrome, it is prescribed. Insufficiency of the corpus luteum is corrected by the appointment of progesterone preparations. Treatment of polycystic ovary syndrome begins with lifestyle changes, diet therapy, normalization of body weight. Metformin is often prescribed to overcome insulin resistance.
In general, the treatment of endocrine forms of infertility is based on the restoration of ovulation. Ovulation is stimulated with the use of hormonal drugs (after establishing the patency of the fallopian tubes). Stimulation of ovulation can be direct and indirect.
Indirect stimulation of ovulation is possible in two ways. Firstly, combined oral contraceptives are prescribed for 3-4 cycles in a row, followed by their cancellation. After stopping the drug, the level of one's own gonadotropic hormones (FSH and LH) rises, as the so-called "rebound effect" develops. Against this background, the likelihood of ovulation and pregnancy increases. Secondly, the use of clomiphene is possible. This drug blocks estrogen receptors, which causes an increase in FSH and LH levels. The lack of sensitivity to the drug is an indication for direct stimulation of ovulation.
For direct stimulation of ovulation, preparations of gonadotropic hormones are used. These include drugs from the urine of menopausal women (menotropins), from the urine of pregnant women, genetically engineered gonadotropins.
In the event that treatment with these methods of hormonal infertility is ineffective, the question of is being considered.
Problems with conception are the result of an unfavorable hormonal background of a woman. And it is not always associated with short-term ailments. Today, doctors are increasingly making a disappointing diagnosis - endocrine infertility. What is this disease?
The collective concept of “endocrine” (or hormonal) refers to several types of disease that are different in their etiology. Their similarity lies in the fact that they are all associated with too low or high content in the female body of thyroid hormones, hypothalamus and pituitary glands, as well as sex glands.

Symptoms of endocrine disorders
The main symptom of the disease is the impossibility of pregnancy. However, there are other symptoms, the combination of which varies depending on the cause of endocrine infertility:
- the complete absence of menstruation or their large delays;
- abnormal course of the menstruation itself (too painful, scanty, abundant, thick, with blood clots);
- severe condition during PMS;
- a normal menstrual cycle is accompanied, which means that we are not talking about menstruation, but about bleeding that mimics them;
- heaviness in the mammary glands and colostrum discharge from the nipples;
- dirty brown discharge in the middle of the menstrual cycle;
- frequent;
- a sharp and inexplicable change in weight (in any direction);
- problems with the skin and hair: the appearance of acne and striae, hypertrichosis, hirsutism, or, conversely, alopecia (hair loss).
The presence of the described symptoms depends on which specific hormones the body has problems with. They are valuable diagnostic signs of endocrine infertility in women.
Causes of hormonal disorders
Depending on the type of “problem” hormones and the pathology of the glands that produce them, there are several key causes of endocrine disorders.
Hyperandrogenism

 This is too high a content in the blood of a woman of male sex hormones, which in small quantities are a prerequisite for the normal development of the female body. This disease can be either primary (congenital) or secondary. In the first case, the excessive production of androgens by the ovaries is genetic in nature. In the second, male hormones are already secreted by the adrenal glands, and this process is provoked by hormone-producing tumors in these glands.
This is too high a content in the blood of a woman of male sex hormones, which in small quantities are a prerequisite for the normal development of the female body. This disease can be either primary (congenital) or secondary. In the first case, the excessive production of androgens by the ovaries is genetic in nature. In the second, male hormones are already secreted by the adrenal glands, and this process is provoked by hormone-producing tumors in these glands.
Sometimes an increased level of androgens is associated with increased work of both the adrenal glands and the ovaries. Often hyperandrogenism is accompanied by polycystic ovaries, overweight, meager periods or amenorrhea, hypertrichosis or alopecia.
Decreased secretion of progesterone and estrogen
If the body lacks female sex hormones, then this is fraught with a change in the state of the endometrium, which transforms and begins to prevent the egg from being transplanted into it. Another consequence of progesterone deficiency is reduced peristalsis of the fallopian tubes. As a result, insufficiency of the luteal phase of the cycle (NLF) is diagnosed.
The causes of this pathology are most often various injuries, previous infections, stress, interrupted pregnancies (both abortions and miscarriages), childbirth with complications, intoxication.
Excess or deficiency of adipose tissue
If there is too little fat in the body or there is an excess of it, then the ovaries suffer primarily, the function of which is impaired. As a result, the menstrual cycle is disrupted, low-quality eggs are produced, which leads to endocrine infertility.
Improper production of thyroid hormones
If there is too much thyroid hormone (hyperthyroidism) or not enough (hypothyroidism), then this can provoke disorders such as:
- anovulation,
- secondary hyperprolactinemia,
- various .
We recommend reading the article about. From it you will learn when it is time to start worrying about the absence of two stripes on the test, what the doctor will prescribe to keep the pregnancy in danger of failure, and also what folk methods and prayers will help in the realization of the cherished dream of having a child.
Genetic pathologies
Gene defects and mutations, chromosomal abnormalities can also cause infertility in women, the symptoms of which often manifest as genital infantilism and primary amenorrhea.
Hypothalamic-pituitary dysfunction
Usually, this pathology is accompanied by hyperprolactinemia, as a result of which the egg simply does not leave the mature follicle due to the depressed function of the ovaries. Factors contributing to the appearance of this pathology are injuries of the skull and chest, tumors in the area of the pituitary gland. The monthly cycle in this case is characterized by the absence of ovulation, and the menstruation itself is characterized by long delays.
early menopause
Another name is emaciated ovary syndrome. The point here is that the content of eggs in the ovaries of a woman is too low. The result is their premature exhaustion and the onset of menopause much earlier than normal for this age.
The presence of severe somatic diseases
With an imbalance in the female body caused by diseases such as tuberculosis, cirrhosis of the liver, cancer, hormone production becomes chaotic, which prevents pregnancy.
These are the causes of infertility in women, the symptoms of which can vary. That is why it is quite difficult to recognize the presence of this serious disease. To make a diagnosis, you should contact a gynecologist, who will conduct a complete diagnosis of the body.
How the problem is diagnosed
At the first visit, the doctor should collect an anamnesis, that is, find out:
- what gynecological diseases the patient suffered earlier;
- whether there were surgical interventions;
- whether there are menstruation, how regular, long and plentiful they are;
- whether there is an experience of pregnancies, as well as their course and outcome (if any).
Next, the metric parameters of the body are examined, such as height and weight (on the basis of which BMI is calculated), the degree of development of secondary sexual characteristics. In addition, the gynecologist will detect the presence or absence of virilism - the presence of male-type hair (mustache, beard, hair around the nipples).
After an external examination, the doctor proceeds to an examination on the gynecological chair, during which he evaluates the metric parameters of the patient's uterus and vagina, the condition of the remaining internal genital organs. Already at this stage, such causes of infertility as or underdevelopment of the genital organs may be revealed.
Additional methods for examining a woman |
What will the test results reveal? |
A woman needs to undergo an ultrasound scan, after which it will become clear if there are any pathologies of the pelvic organs that could not be identified as a result of a gynecological examination. The process of maturation of follicles in the ovaries (folliculometry) is subjected to ultrasound monitoring. In order to find out if the maturation of the egg is taking place, tests are carried out to detect ovulation. Usually, ultrasound monitoring is used for this, but methods such as a urinary test and regular measurement are also informative. Ovulation is also characterized by an increase in the amount of progesterone in the blood, and in the urine - pregnandiol. |
|
Endometrial scraping |
The endometrium of the uterus is also examined, since it depends on its condition whether a fertilized egg can attach to its wall. To do this, two days before the expected menstruation, a scraping of the endometrium is taken. If it is characterized by hyperplasia or secretory insufficiency, then we can talk about the presence of hormonal infertility. |
Examination by an endocrinologist |
The patient is referred for examination by an endocrinologist. The goal is to determine whether the body normally produces hormones such as prolactin, DHEAS and testosterone (androgens), estradiol, LH and FSH (gonadotropins), T4, TSH, T3. If the doctor considers it necessary, then in addition he can prescribe an x-ray of the skull and laparoscopy, as well as send the patient for ultrasound of various endocrine glands. |
In this way, all components of the female reproductive system are gradually explored. Depending on what the main causes of female infertility are, the types of treatment can also be different.
How is endocrine infertility treated?
If during the diagnosis it was revealed that some types of hormones are produced by the body in excess, then drugs are prescribed that reduce this function of the glands. If it turned out that the secretion of the hormone is too low, then, on the contrary, the patient is prescribed hormone replacement therapy or drugs that stimulate the production of deficient substances.
 If endocrine infertility is associated with somatic problems (obesity, the appearance of tumors, the development of diabetes), then these disorders are first corrected. In some cases, even surgery may be required.
If endocrine infertility is associated with somatic problems (obesity, the appearance of tumors, the development of diabetes), then these disorders are first corrected. In some cases, even surgery may be required.
With polycystic ovaries, wedge resection or thermocauterization is most often performed using the laroscopic method.
In each specific case, the set of applied methods of treatment may be different even when the causes of the pathological impossibility of pregnancy coincide. Only an individual and comprehensive approach to therapy can guarantee recovery.
Prognosis for a happy pregnancy with illness
With the modern development of medicine, it is possible to completely cure endocrine infertility in about 80% of all cases. This is a merit not only of gynecologists, but also of endocrinologists. If the reason for the non-occurrence of pregnancy was impaired ovulation, then when this function is restored, women manage to become pregnant already in the first six months after the start of hormone replacement therapy.
The most difficult to treat is hormonal infertility caused by hypothalamic-pituitary dysfunction, but even here the recovery rate is quite high.
As soon as a woman manages to become pregnant, she is shown careful monitoring by a gynecologist and an endocrinologist. At the first suspicion of a threatened miscarriage or premature birth, hospitalization is prescribed. Patients with a history of endocrine infertility are often diagnosed with weak labor activity and discoordination.
Not always the problem lies only in the woman. We recommend reading the article. From it you will learn what types of dysfunction of the male reproductive system are, what signs indicate the presence of a problem, and how the disease is diagnosed and treated if detected.
Prevention of hormonal disruptions
What can cause infertility in women? First of all, these are various diseases of the genital organs and deviations in their work. Therefore, special attention should be paid to the gynecological health of girls, observing all hygiene requirements. If the mother was previously diagnosed with endocrine infertility, regular visits to the pediatric gynecologist and control of the main hormones become mandatory.
Ecology and lifestyle are also very important. You should try to avoid stress, exclude even passive smoking, do not drink alcohol. Proper nutrition will help to avoid weight problems, which also serves as a prevention of hormonal infertility.
Remember that there are no hopeless situations, and infertility is not a sentence for a married couple for a long time. Of course, one should not give up and give up, even if the doctor makes disappointing forecasts. Treat, plan and believe that everything will work out soon! After all, as you know, thoughts tend to materialize!
Content
Endocrine infertility is the most common form of disorganization of the processes of conception. Statistically, half of couples with fertility problems experience this type of disorder. The reproductive system is extremely susceptible to hormonal influence not only from the main regulatory centers, but also from the entire endocrine system as a whole. In fact, any enzyme of the human body, one way or another, has effects on the genital area. Failure of the functioning of one of the endocrine glands can potentially lead to impaired fertilization.
Infertility of endocrine origin: what is it
Endocrine infertility is a symptom complex of hormonal regulation disorders at various levels, leading to the absence of natural conception on the part of both sexes. The mechanism of the disease lies in the perversion of the links between the links of the hypothalamic-pituitary-ovarian system.
Pathology in women is characterized by impaired growth and maturation of the follicle, the absence of a monthly egg release, and a distortion in ensuring the preparation of the endometrium for implantation. Men are more likely to experience an imbalance in the formation of active spermatozoa. As a result, the possibility of fertilization is minimized.
The favorable side is the fact that when a focus of the disease is identified, fertility is restored in most cases. In the absence of results from ongoing endocrine therapy, a married couple can use assisted reproductive technology programs.
Endocrine causes of infertility
Disturbances in hormonal regulation occur at different levels: from brain centers to reserve target tissues. Damage to the central link leads to a decrease in the production of FSH and LH, an increase in the concentration of prolactin. As a result of this influence, the work of the female gonads is perverted.
The block directly in the ovaries forms a persistent estrogen, progesterone deficiency, which forms the impossibility of implantation of the fetal egg. In certain cases, there is damage to the receptor apparatus of the gland. Hormones in this form of infertility are released in the required volume, but the tissues no longer respond properly to the stimulus.
With an increase in the concentration of androgens by the adrenal glands, a persistent block of ovulation occurs: the ovarian cycle stops. Adipose tissue remains a reserve site for the synthesis of hormones. A critical increase or decrease in weight leads to hormonal disorders.
Serious somatic pathologies: hypothyroidism, diabetes mellitus, autoimmune diseases, tumor diseases exacerbate existing metabolic problems. Hormonal imbalance reaches a critical level - conception becomes impossible.
Endocrine infertility in women
Endocrine female infertility develops under the following conditions:
- Dysfunction of the hypothalamic-pituitary apparatus after serious injuries, hemorrhages, tumors, radiation exposure, drug exposure.
- Hyperandronic states due to polycystic transformation of the gonads, diseases of the adrenal glands (Cushing's syndrome).
- Pathology of the thyroid gland.
- Hyperprolactinemia.
- Insufficiency of the second phase of the menstrual cycle.
- Deficiency of female hormones in tumors, inflammatory lesions of the ovaries, accompanied by anovulation.
- Metabolic disorders (anorexia, obesity).
- Syndrome of ovarian resistance.
- Premature menopause.
- Anomalies in the structure of the reproductive system, chromosomal damage.

In men
Infertility among the stronger sex is no less common. As with women, hormonal imbalance causes the most complications in the form of a lack of conception. The causes of endocrine infertility are:
- intrauterine anomalies in the structure of the reproductive organs;
- inflammatory diseases of the sex glands (prostatitis, vesiculitis, orchitis);
- past childhood infections with complications (mumps, brucellosis);
- STI (chlamydia);
- trauma;
- tumors;
- surgical interventions;
- prostate pathology;
- radiation, chemical, drug damage;
- endocrinopathy (diabetes mellitus, hypothyroidism).

Symptoms of endocrine infertility
First of all, an assessment of the constitutional status and development of sexual characteristics is carried out. Endocrine disorders are manifested in the form of an infantile body type, lagging behind, and the absence of secondary reproductive signs. On examination, the specialist evaluates weight, height, type of fat deposition. On the gynecological chair, structural features of the internal genital organs are noted.
The most common signs indicating endocrine infertility include:
- later than menarche;
- violations of menstruation (irregular, scanty discharge, intermenstrual bleeding);
- anorexia or obesity;
- no pregnancy with regular sexual intercourse with no contraception;
- increased hair growth according to the male type (face, hips, chest, white line of the abdomen);
- hirsutism;
- acne
- hair thinning on the head;
- pain in the lower abdomen, lower back;
- secretion of milk from the breast;
- the presence of cysts, tumors of the genital organs;
- artificial termination of pregnancies earlier;
- jumps in blood pressure.
Attention! Bad habits, promiscuity, nervous strain at work further worsen the existing predisposing factors and potentiate the negative impact on the reproductive system - an endocrine type of infertility is formed.
Diagnosis of hormonal infertility
To establish the type and form of endocrine infertility, it is required to establish the concentrations of the main hormones, the change in the level of which leads to infertility. A woman is rated:
- steroids of the menstrual cycle FSH, LH, progesterone;
- prolactin;
- TSH and T4;
- estradiol;
- testosterone, dehydroepiandrosterone and its derivatives;
- adrenal cortisol.
Important! Each hormone is given at strictly defined times of the menstrual cycle. This is an important condition for the correct diagnosis of endocrine infertility.
The main thing is not only to establish the insufficiency or excess of the hormonal background, but also to determine the source. Additionally, gynecologists recommend undergoing the following tests:
- Biochemical analysis of blood taking into account the level of glucose.
- functional tests.
- Ultrasound of the small pelvis in dynamics with the measurement of follicle growth.
- Biopsy of the endometrium.
- karyotype typing.
- Ultrasound of the thyroid gland.
- CT, MRI of the brain.

Treatment of endocrine infertility
Treatment of endocrine infertility directly depends on the cause that contributed to the formation of the condition.
It is necessary to eliminate the negative impact of the root cause of the disease. Traumatic, tumor lesions are removed surgically. Hypothyroidism, diabetes, adrenal pathology are treated according to special schemes, depending on the degree of damage. Be sure to eliminate obesity, underweight.
It is necessary to achieve the growth and maturation of follicles, ovulation. For this purpose, ovulation stimulants are used:
- Clomiphene citrate acts on the pituitary gland and increases the release of FSH.
- Gonadotropins (human menopausal, recombinant follicle-stimulating, hCG). In their chemical structure, the substances are similar to LH, imitate a surge of the latter, and the follicle ruptures.
- Physiotherapy (electrical stimulation of the diencephalic region).
Important! The question of what drug is used to treat infertility of hormonal origin can be answered: everything is strictly individual. In each case, the choice of therapy and dosage is significantly different.
Therapy of endocrine forms of infertility should be carried out by a gynecologist-endocrinologist. The approach to eliminating pathology is complex and requires effort.

Prognosis for endocrine infertility
Hormonal infertility in women can be successfully corrected in 70% of cases. With the restoration of ovulation in the first half of the year, pregnancy occurs in half of the patients. Carrying children to mothers with endocrine disorders carries certain risks. Therefore, such women are necessarily all 9 months under the close supervision of a specialist.
In the remaining cases, when the correction of hormonal disorders has not brought results, there is always a chance of pregnancy with the help of reproductive technologies.
Prevention
To reduce the likelihood of developing pathologies of the reproductive system, leading to endocrine infertility, will help:
- timely treatment of infectious, inflammatory processes of the genital organs, starting from childhood;
- sexual education of teenagers;
- monitoring the formation of menstruation in girls;
- control of body weight within normal limits;
- avoid psycho-emotional, physical overstrain during the formation of the sexual sphere;
- regular visits to the gynecologist;
- correction of hormonal disorders in the early stages;
- correctly selected contraception;
- prevention of unwanted pregnancies (surgical interruption of the first conception increases the development of infertility).
Conclusion
The causes of endocrine infertility predetermine the tactics of treating a married couple. Without the elimination of the main factor leading to hormonal disorders, success cannot be guaranteed. Diagnostic search consists precisely in identifying the source of pathology. Additional normalization of the menstrual cycle with the formation of ovulation makes the process of conception possible.










How to cook frozen cutlets in a pan?
Pike perch baked in salt
How should a girl behave in a relationship with a guy so that he falls in love?
How osteochondrosis manifests itself on an x-ray Visible signs on the human body of osteochondrosis
What can be prepared for the festive table for Easter Easter table decoration and recipes