Up to the 20th century. bacterial infection, such as tuberculosis, meant a death sentence in most cases. Scottish doctor Alexander Fleming discovered in 1928 a substance that causes the death of bacteria - penicillin. However, his works remained unnoticed for a long time.
Systematic studies
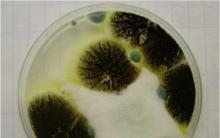
Fleming worked in the bacteriological laboratory of St. Maria in London, from 1928 as a professor. He studied the problem of the growth and properties of staphylococci. The professor was famous for his sloppiness - cups with the remains of bacterial cultures stood unwashed on his desk for weeks. No wonder they eventually grew mold. While looking through the cups before another cleaning, Fleming noticed that there were no bacteria around the mold stains (a common penicillin fungus). The scientist examined penicillium and discovered that the fungus secretes a substance that has bactericidal properties. Fleming named this substance penicillin. Subsequently, it turned out that penicillin is capable of destroying many types of bacteria.
Long road to a cure
Since Fleming never learned how to make penicillin, the discovery did not arouse much interest among doctors. Only in 1939, a team of scientists led by Howard Flory and Ernst Chain managed to isolate pure penicillin from mold and create a world-famous antibiotic on its basis. Clinical trials began in the USA in 1941, and industrial production began in 1944. At first, the new medicine was available only to the Allied armed forces. After the end of World War II, they began to sell it to civilians. In 1945, Fleming, Florey and Cheyne were awarded the Nobel Prize in Medicine.
Bacteria become resistant
Since then, new antibiotics have constantly appeared on the pharmacological market. This is due not only to the love of scientists for experiments, but also to actual necessity: it turned out that
- 1877: Louis Pasteur proclaimed the principle of antibiosis, the impossibility of the existence of some species in the presence of others, later confirmed by the action of antibiotics.
- 1935: The first sulfonamide appeared in pharmacies under the trade name Prontosil.
- 1940: a team of researchers led by American microbiologist Zelman Waksman created the antibiotic streptomycin.
- 1946: Gerhard Domagk developed the first drug against tuberculosis.
If you ask any educated person who discovered penicillin, you will hear the name Fleming in response. But if you look at Soviet encyclopedias published before the fifties of the last century, you will not find this name there. Instead of a British microbiologist, the fact is mentioned that the Russian doctors Polotebnov and Manassein were the first to pay attention to the healing effect of mold. This was the honest truth; it was these scientists who noticed back in 1871 that glaucum suppressed the reproduction of many bacteria. So who really discovered penicillin?
Fleming
Indeed, the question of who and how discovered penicillin requires more detailed study. Before Fleming, and even before these Russian doctors, Paracelsus and Avicenna knew about the properties of penicillin. But they could not isolate the substance that gives the mold its healing powers. Only the microbiologist at St. Hospital succeeded in this. Maria, that is, Fleming. And the scientist tested the antibacterial properties of the discovered substance on his assistant, who had sinusitis. The doctor injected a small dose of penicillin into the maxillary cavity and after three hours the patient’s condition improved significantly. So, Fleming discovered penicillin, which he reported on September 13, 1929 in his report. This date is considered the birthday of antibiotics, but they began to be used later.
Research continues
The reader already knows who discovered penicillin, but it is worth noting that it was impossible to use the product - it had to be purified. During the cleansing process, the formula became unstable, the substance lost its properties very quickly. And only a group of scientists from Oxford University coped with this task. Alexander Fleming was delighted.

But then the scientists were faced with a new task: the mold grew very slowly, so Alexander decided to try another type of mold, simultaneously discovering the enzyme penicillase, a substance capable of neutralizing penicillin produced by bacteria.
USA vs England
The one who discovered penicillin was unable to launch mass production of the drug in his homeland. But his assistants, Flory and Heatley, moved to the United States in 1941. There they received support and generous funding, but the work itself was strictly classified.

Penicillin in the USSR
All biology textbooks write about how penicillin was discovered. But nowhere will you read about how the drug began to be produced in the Soviet Union. There is, however, a legend that the substance was needed to treat General Vatutin, but Stalin banned the use of the overseas drug. In order to master production as soon as possible, it was decided to buy technology. They even sent a delegation to the US Embassy. The Americans agreed, but during the negotiations they raised the price three times and valued their knowledge at thirty million dollars.
Having refused, the USSR did what the British did: they launched a canard that the domestic microbiologist Zinaida Ermolyeva produced crustozin. This drug was an improved one that was stolen by capitalist spies. This was pure fiction, but the woman actually established the production of the drug in her country, although its quality turned out to be worse. Therefore, the authorities resorted to a trick: they bought the secret from Ernst Chain (one of Fleming’s assistants) and began to produce the same penicillin as in America, and consigned crustozin to oblivion. So, as it turns out, there is no answer to the question of who discovered penicillin in the USSR.

Disappointment
The power of penicillin, which was so highly valued by the medical luminaries of that time, turned out to be not so powerful. As it turned out, over time, microorganisms that cause diseases acquire immunity to this drug. Instead of thinking about an alternative solution, scientists began to invent other antibiotics. But to this day it has not been possible to deceive microbes.
Not long ago, WHO announced that Fleming warned about the excessive use of antibiotics, which can lead to the fact that the drugs will not be able to help with fairly simple diseases, because they will no longer be able to harm microbes. And finding a solution to this problem is the task of other generations of doctors. And we need to look for it now.
It is difficult for modern people to imagine the field of medicine without antibiotics. With their help, complex infectious diseases are treated and the lives of millions of people are saved. It seems fantastic that the discovery of penicillin (the first antimicrobial agent) was an accidental occurrence. At the beginning of the 20th century, the scientist Fleming found a fungus, which turned out to be completely harmless to humans, But destructive For malicious microorganisms.
Even at school, we know various stories from the ancient world about the short and fast lives of people. Those who lived to be 13 years old were considered long-livers, but their health was in terrible condition:
- the skin was covered with growths and ulcers;
- teeth rotted and fell out;
- internal organs worked with disturbances due to poor nutrition and excessive physical exertion.
The death of infants was on an alarming scale. The death of women after childbirth was considered common. In the 16th century, human life expectancy was no more than 30 years, and at the beginning of the 20th century, even a small cut could be fatal.
Before antibiotics were invented, diseases were treated in frightening and painful ways.
- In case of infection, bloodletting was indicated (an incision was made in a large vessel or leeches were applied). The goal is to remove blood along with pathogens to the outside.
- Charcoal or bromine was poured onto open wounds to draw out the pus. The patient received a serious burn, but the bacteria also died.
- Mercury was used to treat syphilis. The substance was taken orally or injected into the urethra with thin rods. The only alternative was the even more dangerous arsenic.
History of the discovery of penicillin
The history of the discovery of penicillin, oddly enough, began with the great scientific and technological revolution. In the 19th-20th century, humanity mastered many new areas:
- connection and ;
- radio and entertainment;
- transportation (cars and planes);
- Global ideas for the exploration of the Earth and space began to appear.
But all scientific and technical achievements were overshadowed by people’s everyday life and the most difficult epidemiological situation. Hundreds of thousands of people continued to die en masse from typhus, dysentery, tuberculosis and pneumonia. Sepsis was a death sentence.
Prerequisites for the discovery of penicillin briefly in facts
Many scientists sought to find a solution to the problem and invent an effective cure for ailments. Experiments were carried out, the results of which were usually negative. The idea that special bacteria could kill germs was only introduced in the 19th century.
- Louis Pasteur. Conducted studies that showed that under the influence of certain microorganisms, anthrax bacilli die.
- In 1871, Russian scientists Manassein and Polotebnov discovered the destructive effect of molds on bacteria. But their works were not paid due attention.
- In 1867, surgeon Lister discovered that inflammation was caused by bacteria and proposed fighting them with carbolic acid, the first recognized antiseptic.
- Ernest Duchesne. In his dissertation, he noted that in 1897 he successfully used mold against a number of bacteria that infect the human body.
- In 1984, Metchnikoff used acidophilus bacteria from fermented milk products to treat intestinal disorders.
Who invented penicillin in Russia?
In the Soviet Union, microbiologist Ermolyeva worked on the creation and research of antibiotic drugs. She was the first of all Soviet scientists to begin studying interferon as an antiviral drug. In 1942, Ermolyeva received penicillin. The scientist’s research and experiments led to the fact that within a few years in the USSR the antibiotic began to be produced in large quantities.
Who invented penicillin, Fleming's contribution
 Scientist Alexander Fleming is considered the discoverer of the antibiotic penicillin. For his discovery, the researcher received the Nobel Prize in 1945. The antibiotic appeared by accident: Fleming was sloppy and often did not clean up the test tubes after himself. Before his long absence, the scientist forgot to wash the Petri dishes in which staphylococcus colonies remained.
Scientist Alexander Fleming is considered the discoverer of the antibiotic penicillin. For his discovery, the researcher received the Nobel Prize in 1945. The antibiotic appeared by accident: Fleming was sloppy and often did not clean up the test tubes after himself. Before his long absence, the scientist forgot to wash the Petri dishes in which staphylococcus colonies remained.
Upon arrival, the scientist discovered that mold had bloomed in the cups, and some areas were completely free of bacteria. Fleming concluded that mold produces substances that kill staphylococci. The bacteriologist isolated penicillin from fungi, but was skeptical about his discovery.
Later, scientists Flory and Chain completed the work they started. After 10 years, they improved the medicine and developed a pure form of penicillin.
In 1942, penicillin began to be used to treat people. The first patient to recover was a child with blood poisoning. During World War II, the production of penicillin in the United States was put on an assembly line. Thanks to this, hundreds of thousands of soldiers were saved from gangrene and limb amputation.
How does penicillin work?
The principle of operation of an antibiotic is that it stops or stops the chemical reaction that is necessary to maintain the life of the bacterium. Penicillin stops the activity of molecules involved in the production of new cell layers of bacteria. The antibiotic does not affect humans or animals because the outer membranes of human cells are significantly different from bacterial cells.
 Mechanism and features of action.
Mechanism and features of action.
- Penicillin molecules include bactericidal properties: they have a detrimental effect on a variety of bacteria.
- The main target of action is penicillin-binding proteins. These are enzymes in the final part of bacterial cell wall synthesis.
- When the drug begins to stop synthesis, a process begins that leads to the complete death of the bacterium.
Microbes have learned to defend themselves over time: they began to secrete a special component that destroys the antibiotic. But thanks to the work of scientists, improved drugs that contain inhibitors began to appear. Such antibiotics are called penicillin-protected.
The impact of the discovery on our days
Humanity has gone through a rather complex and confusing path of its development. Many important discoveries and major inventions were made in various fields of activity. Large-scale and decisive discoveries that revolutionized medicine include the creation of penicillin.
Penicillin began to be used on a global scale in 1952. Thanks to its unique properties, it began to be used to treat various pathologies:
- osteomyelitis;
- syphilis;
- pneumonia;
- fever during childbirth;
- infection after wounds or burns.
Later, a variety of antibacterial drugs were isolated. Antibiotics began to be considered a cure for all diseases for many years. Due to the invention of the antibiotic, the fight against serious infectious diseases was improved, and people's lives were extended by 35 years.
September 3 is the official day of the discovery of penicillin throughout the world. For the entire existence of mankind, no other medicine has been invented that would save so many human lives.
Penicillin- a legendary drug. It began the era of antibiotics, which saved millions of human lives. This remedy is still used in the treatment of certain infections. Today it is fashionable to criticize antibiotics, attributing to them all conceivable and inconceivable shortcomings. But with the advent of penicillin, the world changed forever and certainly became a better place.
Who discovered Penicillin?
At the beginning of the 20th century, a means to combat infections became a necessity. The population grew, especially in industrial cities. And with such crowding, any infection threatened a large-scale epidemic.
Scientists already knew a lot about bacteria, the causative agents of the most common and dangerous diseases were isolated and studied, and some drugs were used. But there was no truly effective medicine.
At the end of the 20s of the last century (1881 - 1955), he actively studied pathogenic microorganisms, including staphylococci - the cause of many diseases.
History of discovery
The literature, including fiction, colorfully describes that the Scottish scientist was careless and did not deactivate the bacterial cultures immediately after working with them. And one day he noticed that the growing mold had dissolved the colonies in one of the Petri dishes.
You need to understand that this was not ordinary mold, but brought from a neighboring laboratory. It turned out that it belongs to the genus Penicillium (penicillum). There were doubts about its variety, but experts determined that it was penicillium notatum.
Fleming began growing this fungus in bottles of nutrient broth and conducting tests. It turned out that even with strong dilution, this antiseptic is able to suppress the growth and reproduction of not only staphylococcus, but also other pathogenic cocci (gonococcus, pneumococcus), and diphtheria bacillus. At the same time, cholera virions, typhus and paratyphoid pathogens did not respond to the action of penicillium notatum.
But the main questions were how to isolate a pure substance that destroys bacteria, how to maintain its activity for a long time? - There was no answer to them. Fleming tried to use the broth topically - for treating purulent wounds, for instillation into the eyes and nose (for rhinitis). But massive research has reached a dead end.
In the 40s, attempts to isolate pure penicillin were continued by the so-called Oxford group of microbiologists. Howard Walter Florey and Ernest Chain obtained a powder that could be diluted and injected.
Research was spurred by the Second World War. In 1941, the Americans joined the research and invented a more effective technology for producing penicillin. This medicine was necessary at the fronts, where any wound and even just abrasion threatened blood poisoning and death.
The Soviet government asked the Allies to provide a new medicine, but received no response. Then the Institute of Experimental Medicine, headed by Z. V. Ermolyeva. Several dozen variants of the Penicillium fungus were studied and the most active one was isolated - Penicillium crustosum. In 1943, domestic “penicillin-crustosin” began to be produced on an industrial scale.
This drug turned out to be more effective than the American one. Flory himself visited Moscow to verify this. He, too, wanted to get the original culture of our antibiotic. He was not refused, but was given Penicillium notatum, already known in the West.
Modern concept of antibiotics
Antimicrobial drugs today are divided into many groups. According to the production method they are divided into:
- Biosynthetic - natural - they are isolated from cultures of microorganisms;
- Semi-synthetic - they are obtained by chemical modification of substances secreted by microorganisms.
The classification by chemical composition is widely used:
- β-lactams - penicillin, cephalosporin, etc.;
- Macrolides - erythromycin, etc.;
- Tetracyclines and so on.
Antibiotics are also divided according to their spectrum of action: broad spectrum, narrow spectrum. By predominant effect:
- bacteriostatic - stop bacterial division;
- bactericidal - destroy adult forms of bacteria.
Modern penicillin and natural antibiotics
Today the ancestor of all antibiotics is called benzylpenicillin. This is a β-lactam natural bactericidal drug. In its pure form it does not have a wide spectrum of action. Some types of gram-negative bacteria, anaerobes, spirochetes and some other pathogens are sensitive to it.
Most of the “claims” that people now like to make about all antibiotics can be attributed to natural penicillins:
- They often cause allergies - immediate and delayed reactions. Moreover, this applies to any products that contain penicillin, including cosmetics and food products.
- The toxic effect of penicillins on the nervous system, mucous membranes (inflammation occurs), and kidneys has also been described.
- When some microorganisms are suppressed, others can multiply enormously. This is how superinfections arise - for example,.
- This medicine must be administered in injections - it is destroyed in the stomach. In addition, the drug is eliminated quickly, requiring frequent injections.
- Many strains of microorganisms have or are developing resistance to its action. People who misuse the antibiotic are often to blame.
But it is important to understand that such (and a wider) list of undesirable effects of penicillins appeared thanks to their excellent study. All these disadvantages do not make this drug “poisonous” and do not cover up the obvious benefits that it still brings to patients.
Suffice it to say that all international medical organizations have recognized the possibility of treating pregnant women with penicillin.
To expand the spectrum of action of a natural antibiotic, it is combined with substances that destroy bacterial defenses - β-lactamase inhibitors (sulbactam, clavulonic acid, etc.). Long-acting forms have also been developed.
Modern semi-synthetic modifications help overcome the disadvantages of natural penicillin.
Antibiotics of the penicillin group
Natural penicillins:
- benzylpenicillin (penicillin G);
- phenoxymethylpenicillin (penicillin V);
- benzathine benzylpenicillin;
- benzylpenicillin procaine;
- benzathine phenoxymethylpenicillin.
Semi-synthetic penicillins:
Extended spectrum of action -
Against Pseudomonas aeruginosa -
- Ticarcillin;
- Azlocillin;
- Piperacillin;
Against staphylococcus -
- Oxacillin;
Combined with beta-lactamase inhibitors -
- Ampicillin/sulbactam.
How to dilute penicillin
Whenever an antibiotic is prescribed, the doctor must indicate the exact dose and dilution ratio. Trying to “guess” them on your own will lead to dire consequences.
The dilution standard for penicillin is 100,000 units per 1 ml of solvent (this can be sterile water for injection or saline). Different solvents are recommended for different drugs.
For the procedure you will need 2 syringes (or 2 needles) - for dilution and for injection.
- Following the rules of asepsis and antiseptics, open the ampoule with the solvent and draw the required amount of liquid.
- Puncture the rubber cap of the bottle with penicillin powder with a needle at a 90-degree angle. The tip of the needle should appear no more than 2 mm from the inside of the cap. Add the solvent (required amount) into the bottle. Disconnect the syringe from the needle.
- Shake the bottle until the powder is completely dissolved. Place the syringe on the needle. Turn the bottle upside down and draw the required dose of medication into the syringe. Remove the bottle from the needle.
- Change the needle to a new one - sterile, closed with a cap. Give an injection.
It is necessary to prepare the drug immediately before the injection - the activity of penicillin in the solution decreases sharply.
Penicillium chrysogenium (notatum) is one of the representatives of the genus Penicillium. “Record holder” for penicillin production
The very idea of using other microorganisms (or what they synthesize) to fight microorganisms has been in medicine for a very long time.
In the microbial community itself, some microbes constantly suppress others and are in such a dynamic equilibrium.
Back in 1897, long before the discovery of penicillin, Ernest Duchesne used mold in an experiment to treat typhus in guinea pigs.

Penicillium roqueforti - "noble mold". Used to make Roquefort cheese and gives it its distinctive taste
What do you think guinea pigs, blue cheese and tap water have in common?
The question is quite complicated. It would seem: nothing in common. But if you were a French medical student in the late 19th century, these items would be your scientific reagents.
These reagents were used by the brilliant Ernest Duchesne to discover antibiotics, almost 35 years before Alexander Fleming discovered penicillin.
So the history of antibitics did not begin with Fleming, no. Fleming was not the first to notice the antibacterial properties of mold. Mold was used to treat wounds by the ancient Egyptians. And, although in Ancient Egypt there was no scientific support for many medical actions, we should not forget about the remarkable observation of ancient healers.
Ernest Duchesne
 It was he who first described the antibacterial properties of penicillin. Very little is known about his life. He was born in Paris and studied at the military medical school in Lyon, where he entered at the age of twenty.
It was he who first described the antibacterial properties of penicillin. Very little is known about his life. He was born in Paris and studied at the military medical school in Lyon, where he entered at the age of twenty.
Duchenne was simply fascinated by microbes. Still would! The discovery of pathogenic properties in microbes, the works of Louis Pasteur, simply changed the worldview of doctors of that time. Ernest Duchesne decided to write his dissertation under the guidance of microbiology professor Gabriel Roux. Gabriel Roux then headed the laboratory that was responsible for the quality of the water supply in Lyon. Duchesne's thesis focused on the following observation: tap water never became moldy, but mold could grow well in distilled water. The first suggestion was that bacteria prevented mold from growing in tap water.
Ernest grew Penicillum glaucum. This mold is used to make Gorgonzola and Stilton cheeses. He placed it in containers with tap and boiled water. Then he added the causative agent of typhoid fever and E. coli - the mold quickly died. It turned out that bacteria in water kills mold. Duchesne began to set different conditions: temperature, acidity of the environment, but the mold did not always die. Sometimes victory remained with the fungus.
The question arose again: can mold “answer” bacteria in some way? Can she fight them? An experiment on guinea pigs revealed a decrease in bacterial virulence. Moreover, by injecting mold, Duchesne was able to cure the animal. A similar experiment will be carried out by Alexander Fleming, who is often called the discoverer of penicillin.
A lot has been written about how penicillin was discovered by Fleming. So why isn't Duchenne remembered as the discoverer of penicillin? There are several reasons for this. Well, first of all, he studied Penicillum glausum, as opposed to another type of mold, Penicillum notanum. The mold that actually synthesizes this penicillin. Later it was found that Penicillum glausum produces another, weaker antibiotic - patulin (by the way, it is toxic and works in high concentrations, so it is not used). Probably, if not for the health of the young scientist, as well as his short life (he died of tuberculosis in 1912, having lost his wife from the same tuberculosis long before), the discovery of penicillin would have been his.
Alexander Fleming
 But a fact is a fact. The author and discoverer of penicillin was Alexander Fleming. The date of discovery of the most famous antibiotic is September 3, 1928 (the birthday of penicillin). Fleming by that time was already widely known and had a reputation as a brilliant researcher.
But a fact is a fact. The author and discoverer of penicillin was Alexander Fleming. The date of discovery of the most famous antibiotic is September 3, 1928 (the birthday of penicillin). Fleming by that time was already widely known and had a reputation as a brilliant researcher.
Humanity still owes the discovery of penicillin to this Scottish biochemist. After World War I, in which the “father of penicillin” served as a military doctor, Fleming could not come to terms with the fact that a large number of soldiers were dying from infectious complications. In 1918, he returned from the war to work in the bacteriological laboratory of St. Mary's Hospital, where he had previously worked (and where he would work until his death). In 1922, an incident occurred that was, of course, more like a fable, but nevertheless preceded the discovery of penicillin by six years. Fleming, who had a cold, accidentally sneezed onto a Petri dish containing bacterial colonies. After a few days, he discovered slow growth of bacteria (Micrococcus lysodeikticus) in some areas. This is how lysozyme (muramidase) was discovered. This hydrolytic enzyme breaks down the walls of bacteria, that is, it has bactericidal properties. There is a lot of it in nasal mucus, saliva (why animals can lick wounds), tear fluid. There is also a lot of it in breast milk (and noticeably more than in cow’s milk, and with feeding, its concentration does not decrease over time, but increases). Of course, when penicillin is discovered, interest in lysozyme will noticeably drop, until the discovery of chicken protein lysozyme.
As Alexander Fleming himself later noted, the discovery of penicillin was helped by chance. Working in the laboratory and studying the enzyme lysozyme, Fleming was not distinguished by order in the workplace (although scientists have their own order!). As is often the case with geniuses (just remember Einstein’s desk), the scientist’s laboratory was a complete mess. Fleming, returning after a month of absence, noticed that mold fungi had appeared on one plate with staphylococcus cultures. A colony of fungus dissolved the sown crop. The mold belonged to the Penicillium genus, which is why the isolated substance was later called penicillin.

The name of penicillin translates as “writing brush”, such a similarity is visible under a microscope
Howard Flory
 And although when it comes to the discovery of penicillin, Alexander Fleming is remembered, other scientists, in particular the pharmacologist Govrad Walter Flory, benefited from this discovery. In 1938, Florey, working with Ernest Chain and Norman Heatley at Oxford University in England, began experimenting with the antibacterial properties of the fungus Penicillium notatum. Fleming wrote about the properties of the fungus to suppress bacterial growth in his works.
And although when it comes to the discovery of penicillin, Alexander Fleming is remembered, other scientists, in particular the pharmacologist Govrad Walter Flory, benefited from this discovery. In 1938, Florey, working with Ernest Chain and Norman Heatley at Oxford University in England, began experimenting with the antibacterial properties of the fungus Penicillium notatum. Fleming wrote about the properties of the fungus to suppress bacterial growth in his works.
The first patient to be prescribed penicillin was Albert Alexander, a London policeman. The serous infection, which affected part of the face, the periorbital area of the eye, and the scalp, began with a small prick from a rose thorn. Flory and Chain gave the patient penicillin and during the first 24 hours good dynamics were observed. However, it was not possible to determine the optimal dose of the drug (it was not known at that time) and the infectious process still led to the death of the patient. Experiments continued, and the drug was administered to seriously ill children with impressive results. It is now believed that the work of Florey and Cheyne saved more than 80 million people.
Ernest Cheyne
 And now it’s worth mentioning the previously mentioned biochemist Ernest Boris Chain. Born into a Jewish family and living in Germany, he was forced to emigrate to England when Hitler came to power. As a joint recipient of the future Nobel Prize for the discovery of penicillin, Cheyne was awarded that part of the work in which he showed the structure of penicillin and successfully isolated the active substance. To isolate penicillin for one therapeutic dose, it was necessary to process about 500 liters of nutrient broth with mold!
And now it’s worth mentioning the previously mentioned biochemist Ernest Boris Chain. Born into a Jewish family and living in Germany, he was forced to emigrate to England when Hitler came to power. As a joint recipient of the future Nobel Prize for the discovery of penicillin, Cheyne was awarded that part of the work in which he showed the structure of penicillin and successfully isolated the active substance. To isolate penicillin for one therapeutic dose, it was necessary to process about 500 liters of nutrient broth with mold!
Cheyne wrote: “The difficulties Fleming encountered only fueled my interest in Fleming’s discovery of penicillin. I told Flory that we would find a way to at least partially purify penicillin, despite its instability.”
In 1938, Chain and his colleague Norman Heatley quickly came to the conclusion that penicillin, unlike lysozyme, was not an enzyme but a small molecule of organic origin.
The small size of the molecule gave researchers hope that it would be easy to decipher the molecular structure and synthesize it. Scientists were wrong about how easy it would be...
It was found that penicillin contains a complex of structures that were later called beta-lactams. 
Cheyne had previously suggested the possibility of the existence of such a structure, but the issue was resolved only in 1949.
 When, using X-ray crystallography, Dorothy Hodgkin determined the arrangement of atoms in the crystal lattice of penicillin. It was after 1949, after the precise molecular structure of penicillin was determined, that mass, cheap production of the drug became possible.
When, using X-ray crystallography, Dorothy Hodgkin determined the arrangement of atoms in the crystal lattice of penicillin. It was after 1949, after the precise molecular structure of penicillin was determined, that mass, cheap production of the drug became possible.
By the way, Dorothy Hodgkin also received the Nobel Prize for her study of crystal lattice in X-rays in 1964. This outstanding woman laid the foundations of the method that made it possible to study the structure of DNA (the Human Genome Program).
Chain and Flory used a then new lyophilization technique to obtain penicillin in concentrated form. The penicillin solution was frozen and then, at low temperature and low pressure, the water was expelled, leaving behind the valuable material.
Penicillium chrysogenium (notatum): how the most “penicillin” fungus was found
Since the beginning of World War II, the need for penicillin has increased dramatically. The need for such a medicine was obvious.
In 1940, a group of scientists at Oxford University (led by Florey and Chain) took Fleming's penicillin out of storage and began to look for ways to produce it in large quantities.
Since the bombing of London began and the risk of occupation arose, the scientists went to negotiate in New York (the likelihood of a German landing was so great that Chain even soaked his jacket with healing mold, explaining to his colleagues: if something happened, save this jacket first).
In New York, visiting scientists were greeted without much enthusiasm: the production of penicillin rarely exceeded 4 action units per 1 milliliter of nutrient medium. This is very little: on a bottle of penicillin, for example, it says “1,000,000 units.” For one dose of the drug it was necessary to process 250 liters of broth.
The goal immediately became clear: to find the most “fruitful” fungus. First, the scientists went to Peoria, Illinois, where there was a research laboratory studying mold metabolism. The laboratory staff collected a significant collection, but only a few strains of mold could produce penicillin.
We started inviting friends to send us samples of soil, mold grains, fruits and vegetables. They hired a woman to go around stores, bakeries, and cheese factories, looking for new samples of blue-green mold. Her name was Miss Mary Hunt, nicknamed "Mouldy Mary" for her good work.
The course of history was changed by the cantatula melon, on which a blue-green fungus settled. This mold produced 250 units of penicillin per milliliter of growth medium. One of the strains that mutated from it began to produce 50,000 units! All strains that produce penicillin today are descendants of the same mold that was found in 1943. It was the fungus Penicillium chrysogenium, formerly called Penicillium notatum.
From that moment on, the era of industrial production of penicillin began.
When Fleming, Florey and Chain were awarded the Nobel Prize in Physiology or Medicine in 1945, Fleming said: “They say that I invented penicillin. But man could not invent it - this substance was created by nature. I didn’t invent penicillin, I just drew people’s attention to it and gave it a name.”.

Fleming, Chain and Florey at the Nobel Prize ceremony
If you find a typo in the text, please let me know. Select a piece of text and click Ctrl+Enter.










Red Book of the Leningrad Region Three-toed woodpecker - Picoides tridactylus
Humanitarian Institute named after
Krasnoyarsk State Pedagogical University named after V
Identifying relative clauses and Non-identifying relative clauses
Russian-English translation joint purchase Expressions and idioms about shopping